Abstract
Intro: APL is one of the most curable forms of acute myeloid leukemia. Whereas all-trans retinoid acid (ATRA) and arsenic trioxide (ATO) are the standard of care for treatment of low/intermediate risk APL (APL0406 trial, LoCoco et al. NEJM 2013), the optimal treatment of high-risk APL remains unclear. In our institution, we use the APML4 regimen (Iland et al. Blood 2012) to treat high-risk APL patients, which uses idarubicin+ATRA followed by ATRA+ATO for induction. Then, there are two consolidation cycles of ATRA+ATO, the first of which is 28 consecutive days of treatment. Consolidation is followed by two years of ATRA + 6-mercaptopurine + methotrexate maintenance (PETHEMA LPA99, Sanz et al. Blood 2003). In the APML4 trial, the outcomes were excellent for all risk groups, particularly for high-risk patients. However, this regimen cannot be administered in community infusion centers (CIC) that are not open on weekends. In addition, the expertise required to give maintenance therapy makes it challenging to administer outside of an academic medical center. Here, we examine outcomes of high-risk APL patients who received induction at our institution to document the types of consolidation regimens they received and their outcomes. In particular, we focus on the outcomes of high-risk APL patients who received induction with idarubicin+ATRA+ATO (as per APML4) at our institution, and then for practical considerations received consolidation with ATRA+ATO (as per APL0406) in the community.
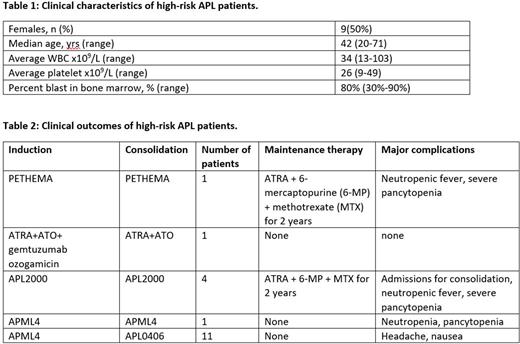
Methods: We performed a retrospective analysis of all patients between the ages of 18-89 who were diagnosed with high-risk APL at the Knight Cancer Institute between January 2009 and July 2022. We identified 19 patients with the diagnosis of high-risk APL. One patient died soon after diagnosis due to intracranial bleed (excluded from final analysis). The remainder completed induction and consolidation.
Result: Table 1 shows the main clinical features at diagnosis. The most common complications during induction were differentiation syndrome and coagulopathy. All 18 patients achieved complete morphologic remission (CR) at the end of induction but still had detectable PML-RARA by PCR. 4/18 (22%) patients received the APL2000 regimen (Adès et al. JCO 2006), and 1/18 (6%) patient received the PETHEMA regimen (Sanz et al. Blood 2003). All 5 patients were hospitalized for neutropenic fever, which required significant dose reduction and treatment delay. One patient (6%) received induction with ATRA+ATO+gemtuzumab ozogamicin followed by consolidation with ATRA+ATO (Estey et al. Blood 2006). The majority of patients (12/18, 67%) received induction as per APML4 protocol (Table 2). The APL0406 regimen was administered as consolidation in 11/18 (61%) patients; and all patients except one received consolidation at local CIC. Common side effects were headache and nausea, leading to dose reduction in five patients. One patient continued with APML4 consolidation. Molecular CR was confirmed in all patients at the end of consolidation treatment. 13/18 (72%) patients did not receive maintenance therapy after consolidation. All patients were subsequently followed by RT-PCR for PML/RARA for molecular relapse. At the last follow up, all 18 patients remained to be in molecular CR with no relapsed disease.
Discussion: The benefit of ATRA+ATO for low/intermediate risk APL patients is well established, but the optimal management of high-risk APL remains a challenge, especially when consolidation is given in CIC. Our series of patients provides real world evidence that ATRA+ATO consolidation as per APL0406 regimen is effective in high-risk APL patients after induction with idarubicin+ATRA+ATO as per the APML4 regimen. Although the numbers are limited, all patients remain in molecular remission as measured from the end of consolidation, similar to the excellent outcomes of low/intermediate risk APL patients. Consolidation was well tolerated, with minimal treatment delays, suggesting that a standard consolidation regimen for low-, intermediate-, and high-risk APL patients can be successfully administered in the community (most centers typically treat 1-2 patients per year with APL). The majority of patients did not receive maintenance therapy but remained in remission, providing further evidence that maintenance therapy is unnecessary with sufficient ATRA+ATO consolidation, and simplifying therapy (Shah et al. Blood 2018).
Disclosures
No relevant conflicts of interest to declare.
Author notes
*Asterisk with author names denotes non-ASH members.